Prior Authorization Agent
Cut delays. Reduce denials. Accelerate clean claims
Built on the Caregence platform, the Prior Authorization Agent automates the entire prior auth process—capturing data, identifying payer channels, and tracking status in real time. The built-in browser agent navigates payer portals, fills forms, attaches documents, submits claims securely, and updates your system of record
The problems it fixes
High denial rates
Manual errors and shifting payer rules trigger avoidable denials. Every rejection creates rework and slows care

Heavy administrative burden
Providers and staff spend 13 to 14 hours each week on forms and follow-ups that pull time away from patients.
Long approval timelines
Approvals often take 10 to 14 days. Delays force reschedules and increases the risk of treatment abandonment
Fragmented systems
EHRs, CRMs, payer portals, and fax workflows do not connect cleanly. Staff bridge gaps with copy-paste and re-entry.
Patient impact
Delays harm outcomes and trust. Many physicians report patients sometimes abandon treatment when approvals stall.
What the prior authorization agent does

Instant data capture
Pulls patient, payer, provider, and clinical context from your EHR and CRM. Auto-fills authorization forms. No manual typing.

Seamless payer access
Chooses the best route per payer: portal, API, phone assist, or fax.

Real-time status + resubmission
Tracks every request, posts updates in your work queue, and auto-prepares resubmissions with corrected documentation.

Actionable oversight
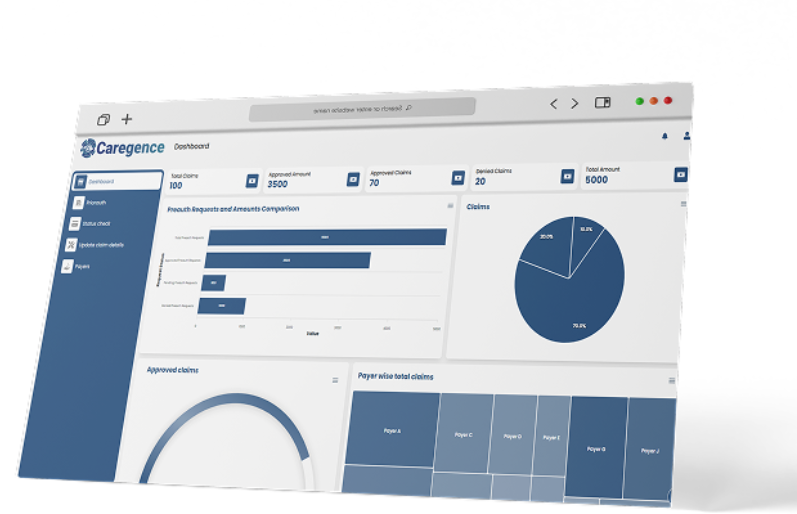
Live dashboards show volume, time-to-decision, denial reasons, and predicted risk. Managers can intervene early.
How it works on the Caregence platform

Data capture
- Reads demographics, coverage, diagnosis, CPT/HCPCS, clinical notes, and prior history.
- Validates fields and codes, flags missing documentation, and fills payer forms automatically.

Documentation and write-back
- Writes benefits, auth numbers, decisions, and timestamps back to the EHR.
- Maintains a clean audit trail for compliance and appeals..

Verification routing
- Selects the optimal channel per payer and program based on historical success and current rules.
- Handles benefit checks and medical necessity criteria before submission.

Submission and tracking
- The browser agent takes over here, auto-populating payer-specific forms, attaching required documents, and submitting the prior authorization request for approval.
- Submits documentation bundles and monitors status in real time with reminders and escalations.
Outcomes you
can expect
Salient features
Comprehensive, Secure, and Intelligent Prior Authorization Agent
Works across EHR, CRM, scheduling, and imaging systems
Payer playbooks that update as rules change
HIPAA-aligned processing with role-based access
Document OCR and field-level validation for IDs, orders, and notes
Appeals kit generator with reason codes and required attachments
Full audit logs and exportable packet history
FAQs
Can we keep our current payer portals?
Yes. The agent uses the best available route per payer, including your existing portals and APIs.
How do updates to payer rules get handled?
Playbooks are updated centrally. Changes roll out without rebuilding your workflows. Any changes to the workflow on payer portals are handled by agents automatically without any human intervention.
Do clinicians have to learn a new tool?
No. Tasks and updates can be integrated in the systems you already use. Alternatively, a simple dashboard can be provided to trigger and monitor the tasks and updates.
Can this help with claim appeals?
Yes. It assembles claim appeal packets associated with the right reasons and codes with supporting documentation.
Make prior authorization work for you
See how the Prior Authorization Agent speeds approvals and cuts denials.